
Frailty virtual wards: 4 key elements of success
In recent years, the NHS has placed a focus on implementing frailty virtual wards to help care for patients without the need for hospital admission. As a result, virtual wards can, and have been proven to, reduce ED admissions and unplanned hospital admissions within care settings. With the right approach, ICSs can continue to provide the same level of care for their patients whether they’re at home or on the ward. In this article, we’ll explore frailty wards in more detail and the key elements of a successful virtual care system.

What is a frailty virtual ward?
A frailty virtual ward is a dynamic and responsive model of care designed to address the specific needs of frail patients. Operating outside the traditional hospital setting, these virtual wards aim to provide holistic care through a system-wide approach, personalised patient pathways, and the integration of innovative technology to facilitate at-home monitoring. According to the NHS, around 86% of ICSs have either implemented technology-enabled virtual wards or are planning to do so in the near future, thanks to their ability to transform patient care and reduce unnecessary burdens on staff.
In general, a virtual ward is a time-limited provision of care for people with an acute condition or worsening chronic condition that requires hospital-level care. With a virtual ward, these patients can continue to receive the care they need at home or elsewhere in the community, both as an alternative to hospital admission and to enable earlier discharge. For frailty patients in particular, virtual wards can significantly reduce the risk of contracted diseases and further illness posed by admission to hospital.
Both step-up and step-down models of care use virtual wards to provide coordinated patient care. Step-up models can use virtual wards as an alternative to admitting patients to hospital, helping to avoid unnecessary admissions. While step-down models of care can use virtual wards to enable early discharge and provide care at home for patients with conditions that would otherwise have required admission to the hospital ward.
Although out-of-hospital care, virtual wards can still deliver hospital-level treatment, including monitoring of vital signs and real-time health data analysis. Virtual wards are often a combination of remote and face-to-face care, requiring a collaborative approach between acute, primary, and community care across an ICS. These cohesive efforts of virtual ward nurses and integrated care systems ensure that patients receive timely interventions, adjustments to care plans, and ongoing support as and when they need it.
The Key Elements of a Frailty Virtual Ward
For a virtual ward to be successful, it requires a collaborative effort between care providers with personalised, acute-level care for patients catered to their individual needs. As the NHS specifies, this relies on a multi-disciplinary approach that establishes clear lines of communication, criteria for care, and integration with other care services.
A system-wide approach
Frailty virtual wards adopt a holistic, system-wide approach that involves collaboration between various healthcare professionals. This means bringing together professionals across acute, primary, and community pathways to address the multifaceted needs of frailty patients, ensuring that all aspects of their wellbeing and needs are considered.
To establish this system-wide approach, virtual wards should be delivered by a multidisciplinary team (MDT), that includes clear lines of responsibility and governance. This includes creating partnerships between various staff, from AHPs and advanced nurse practitioners to GPs, who all work together towards one goal – facilitating the patient’s care. Typically, the virtual ward should be led by one clinical practitioner with relevant experience who can ensure resources are used effectively and that the virtual ward is running successfully. It should also build upon existing systems and pathways in place to advance care, such as rapid response teams.
Patient-centric pathway
It’s critical to ensure frailty virtual wards cater to the individual needs of every patient. This means bringing together healthcare professionals from different specialisms to facilitate a care plan, whether that’s emotional support or remote monitoring of vital signs. As such, virtual ward teams should carefully consider the information and questions provided on a virtual ward pathway to encourage patients to provide the data needed to coordinate care.

If a patient’s symptoms worsen during out of hours, they should be well aware of who to contact to receive the care they need. Likewise, if a frailty patient would be considered at higher risk alone at home, it may, in some cases, be more suitable to escalate their care to the hospital or a care home where staff are on hand to support them.
Teams must also establish set criteria for who they will and will not treat. This should be part of a wider discussion around local and geographical needs. Importantly, virtual wards should not be used as a gateway service for any and all elderly patients outside of a hospital setting. As a result, it’s important to define the criteria for admission to the frailty virtual ward, as well as how to determine if a patient can be discharged or, if needed, stepped up to hospital admission.

Technology-enabled patient care
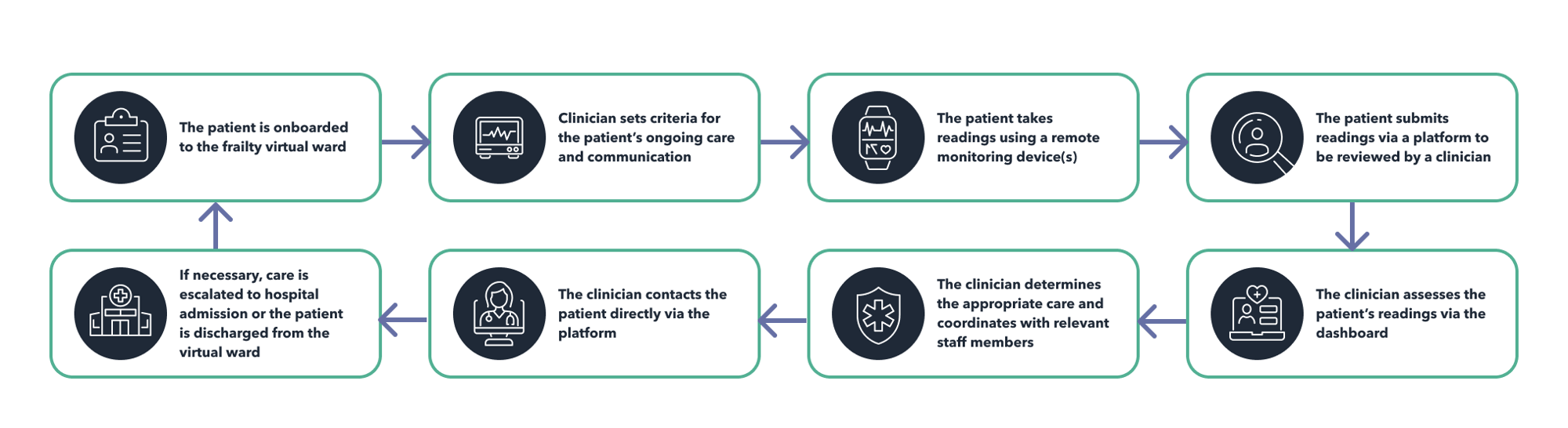
As the NHS outlines, virtual wards should be fully technology-enabled to enable patient care and effective management of their condition. Clinical teams should take advantage of available technology, including remote monitoring devices, ultrasound and diagnostic devices, wearable sensors, and smart home applications that patients can use to gather data about their condition and, if necessary, submit readings to a platform.
Clinical teams can then monitor these platforms to evaluate patient health and coordinate any healthcare provisions as and when needed. They can communicate with patients via the platform to provide necessary care advice, rather than encourage unnecessary ED admissions.
However, teams must also consider issues around digital exclusion and accessibility to devices. For frailty patients especially, staff must provide appropriate onboarding and training for patients to ensure they know how to use their devices correctly for them to receive the best possible care.
Clearly-defined impact measures
Evaluation is necessary to assess the impact and effectiveness of the frailty virtual ward, not just for reducing hospital admissions, but also for improving the lives of patients in your care. It’s important to establish clear and regular touch points for assessing impact, as well as to define how impact will be measured.
This typically combines qualitative and quantitative data, gathering information about ED admissions, unplanned admissions, improvements in patient-reported outcomes, utilisation of hospital beds, and cost factors. It also involves gathering feedback from staff, patients, and patients’ families to evaluate the virtual ward model and make improvements where necessary.
Facilitating at-home frailty care
Frailty virtual wards are emerging as a transformative force in healthcare, providing a patient-centric, technology-enabled approach to out-of-hospital care. To ensure success, frailty virtual wards must be driven by a system-wide approach that brings together multidisciplinary teams within ICSs. Care must be patient-centric, understanding the uniqueness of each frailty patient and how best to escalate and coordinate their care. The use of remote monitoring devices is pivotal in this care pathway, enabling healthcare professionals to monitor patients’ conditions without the need for hospital admission.
At Luscii, we’re passionate about remote care. Luscii is the system-wide platform for healthcare at home, enabling UK ICSs to better connect the dots between acute, primary, and community care. Our remote monitoring platform is used within NHS trusts throughout the UK, facilitating care for various long-term and acute conditions, including frailty patients. Learn more about our frailty pathway and watch our webinar to see how we can help you successfully implement virtual wards for your patients.
Want to hear more about Luscii?
Luscii is the system-wide platform for health care at home. Luscii's innovative remote monitoring pathways connect the dots between acute, primary, and community care. Our clinically-proven programs enable healthcare establishments across the UK to reduce unplanned admissions, lower A&E attendances, cut costs, and deliver faster discharge.